A 22 year old woman presented to our outpatient unit with the complaints of
Bilateral lower limb swelling since 1 month
Facial puffiness since 1 month
Shortness of breath since 1 month
Reduced urine output since 1 week
History of present illness :
1 month back, she first noticed bilateral lower limb swelling, pitting type upto her ankles which gradually extended to her thighs. Following this she also developed facial puffiness, significantly around her eyes which alarmed her and she paid a visit to our hospital and was started on conservative medications. However her symptoms did not subside. She started experiencing dyspnea on exertion which gradually progressed to an extent that she found it difficult to even walk for a short distance. She reported frothing of urine, however she had no hematuria. She complaints of reduced urine output since 1 week.
She did not have any history of chest pain, palpitations, giddiness, sweating.
She denied any history of fever, sore throat, rash, joint pains. No history of drug intake or antibiotic usage.
Past History:
12 years back, she was diagnosed with Type 1 Diabetes Mellitus on visiting a local hospital for fever and body pains. She has been receiving insulin injections since then.
In 2018, she was admitted in a local hospital for slurred speech which eventually became normal on normalising her blood sugar levels.
Her father reported that she had to be readmitted 2-3 times there after with the same complaints of slurred speech and hyperglycaemia. She was started on Injection Human Insulin Mixtard 18 units in the morning and 12 units at night.
6 months back, she was diagnosed with Hypertension on routine follow up and was started on Tab Telma 40mg once daily.
4 months back, she had an abortion at 7 weeks of gestation since the fetal heart beat couldn’t be assessed.
Personal History:
She currently lives with her parents who work as daily wage laborers. She has 2 elder sisters, who are married. She studied till 10th standard. She was married 1 year back to a farmer, however they haven’t been living together ever since her miscarriage.
Her mother reported decreased appetite since the last 2 months. She has only been consuming only milk, once to twice a day along with chapatti once in a day.
Problem Representation:
1. Generalized Anasarca
2. Dyspnea on exertion
3. Reduced urine output
4. Uncontrolled blood sugars
Provisional Diagnosis:
1. A 22 year old woman with significicant generalized anasarca, proteinruria and hypertension - Nephrotic Syndrome - ? Diabetic Nephropathy
2. Anemia secondary to ? chronic disease
3. Type 1 Diabetes Mellitus since 12 years
4. Hypertensive since 6 months
Clinical Examination:
General Examination:
Pulse Rate: 90 beats per minute, normal on volume, no radio-radial or radio-femoral delay
Blood Pressure: 150/70mmhg, right arm, supine posture
Respiratory Rate: 22 cycles per minute
Temperature: 98.6 F
Spo2: 98% on Room Air
GRBS: 260mg/dl
Height: 152.4 cm
Weight: 58 kgs
Body Mass Index: 23.2 kg/m
Waist circumference: 96 cms
Images from previous admission:
Current admission pictures:
Head to toe:
Hair: Normal colour and texture, No areas of hair loss.
Eyes:
Pallor +
Periorbital edema +
Bilateral pterygium +
No cyanosis, icterus
Right IJV central line:
Left thigh hyperpigmented lesion present since her childhood,? Acquired nevus
Bilateral lower limb edema, comparatively reduced due to Hemodialysis
Systemic Examination:
Abdomen:
Inspection:
Distended
Umbilicus - Slit like
No visible scars, sinuses, pulsations
Palpation:
No tenderness
No guarding or rigidity
No palpable masses
No organomegaly
Percussion:
Shifting dullness couldn't be elicited
Auscultation:
Bowel sounds +
Nervous System Examination:
Only positive findings mentioned:
Optic Nerve -Fundoscopy
Right eye: Nonproliferative Diabetic Retinopathy
Left eye: Proliferative Diabetic Retinopathy
Respiratory System Examination:
Right infrascapular crepts + on auscultation
Cardiovascular System Examination:
S1, S2+
Investigations:
ECG showing
Heart Rate of 100 beats per minute
Left Axis deviation
Low voltage complexes
Poor R wave progression
Chest Xray PA view:
Showing:
Left side breast shadow
Left pleural effusion
Right IJV central line +
Showing normal sized chambers
with an ejection fraction of 60 %
Concentric LVH
Pericardial Effusion +
Fasting Lipid Profile:
Total cholesterol - 247mg/dl
Triglycerides - 262mg/dl
HDL - 48 mg/dl
LDL - 110 mg/dl
VLDL - 52.4 mg/dl
24 hours urinary protein : 2600mg/day
From the day of admission:
Fasting Lipid Profile:
Total cholesterol - 247mg/dl
Triglycerides - 262mg/dl
HDL - 48 mg/dl
LDL - 110 mg/dl
VLDL - 52.4 mg/dl
Diagnosis:
1. Diabetic Nephropathy with eGFR of 17.5 ml/min/1.73 m and creatinine clearance of 24 mL/min
Diabetic Retinopathy -
2. Anemia secondary to chronic disease
3. Type 1 Diabetes Mellitus since 12 years
4. Hypertension since 6 months
Discussion:
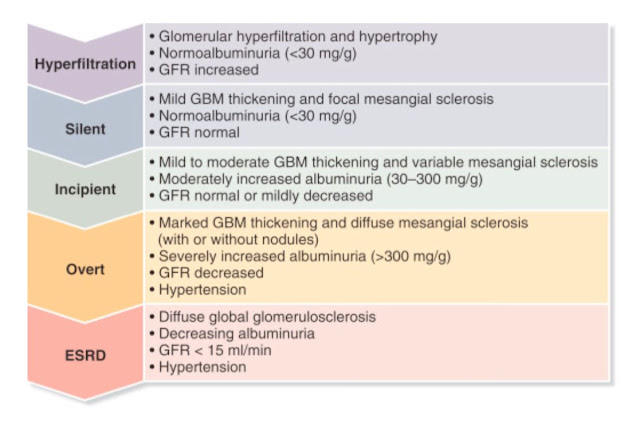
Stages of Diabetic Nephropathy
Earlier identification of GFR decline would allow interventions to decrease the rate of GFR loss and prolong the time to development of end stage renal disease (ESRD)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4138314/#!po=8.46154
Critical Appraisal:
Dual blockade of the renin–angiotensin system in type 1 patients with diabetic nephropathy
P - 21 type 1 patients with Diabetic Nephropathy
DN was diagnosed if the following criteria were fulfilled: persistent albuminuria >300 mg/24 h in two out of three consecutive determinations, presence of diabetic retinopathy, and no clinical or laboratory evidence of other kidney or renal tract disease
I - Each patient received 2 months of treatment with Irbesartan 300 mg o.d.
C - 2 months of placebo.
The study medication was added on top of the patient's usual antihypertensive treatment.
O -


O - Our short‐term study suggest that dual blockade of the RAS offers additional renal and cardiovascular protection in type 1 patients with diabetic nephropathy.
If you notice from my perspective, there’s not much of a difference between both the groups
Cons: Also, 2 months assessment of the effect of Irbesartan wouldn’t be sufficient. We need to assess the long term effects.
The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus
P - A total of 1441 patients with IDDM -- 726 with no retinopathy at base line (the primary-prevention cohort) and 715 with mild retinopathy (the secondary-intervention cohort)
I - 1441 were assigned to intensive therapy administered either with an external insulin pump or by three or more daily insulin injections and guided by frequent blood glucose monitoring or to conventional therapy with one or two daily insulin injections. The patients were followed for a mean of 6.5 years, and the appearance and progression of retinopathy and other complications were assessed regularly.
According to this the patients on intensive phase reduced risk of diabetic retinopathy, only 23 patients developed diabetic retinopathy and 91 patients on conventional therapy developed retinopathy.
In the two cohorts combined, intensive therapy reduced the occurrence of microalbuminuria by 39 percent, that of albuminuria by 54 percent, and that of clinical neuropathy by 60 percent.



.jpeg)
.jpeg)


.jpeg)













.jpeg)




.jpeg)
.jpeg)
No comments:
Post a Comment